New mobile health technology for sleep apnea care to address individual patient needs

Sleeping with a Continuous Positive Airway Pressure, or CPAP, machine is the most effective treatment for sleep apnea, yet getting patients to use the devices consistently remains a major challenge. Now, a development by University of Chicago Medicine and Northwestern University scientists gives both patients and physicians a new tool for monitoring adherence to therapy.
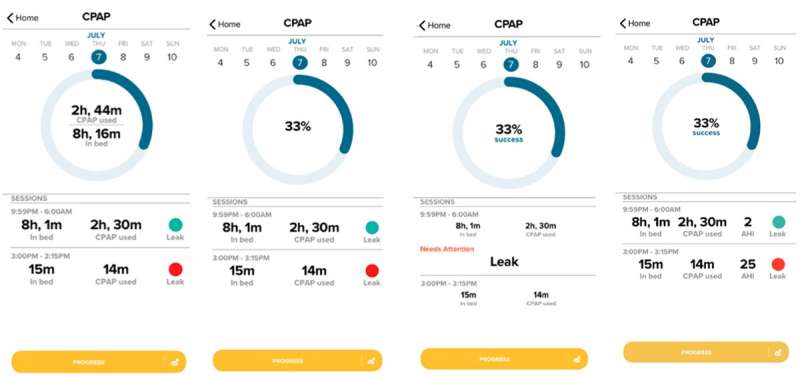
For the study, researchers designed an app to track CPAP use, along with sleep tracking and other health metrics. The idea behind the design is simple: Although current guidelines describe at least four hours of CPAP use per night as adequate, the researchers argue that the amount of therapy that patients need varies from person to person nightly because it should align closely with how many hours they sleep.
“Sleep apnea can be effectively treated only when CPAP is used during the entire time spent in bed sleeping,” said Esra Tasali, MD, Director of the UChicago Sleep Center and senior author of the paper. “We know that sleep patterns can vary considerably, so one-size-fits-all adherence guidelines are insufficient for most patients. By developing a tool for personalized CPAP treatment for sleep apnea, we are providing an opportunity for patients and providers to deliver and track therapy based on individual need.”
The research was published in the Journal of Medical Internet Research.
CPAP needs vary person to person
The tool provides a new adherence metric: the percentage of time a user wears their CPAP relative to their objectively assessed time spent sleeping. This allows therapy to be customized to the patient’s needs every night. The new metric provides markedly different information on adherence success as compared to traditional CPAP tracking methods that simply report how many hours a CPAP mask was worn without accounting for the time slept without it.
Sleep apnea affects an estimated 54 million American adults and 1 billion people worldwide. Left untreated, sleep apnea has been linked to serious health conditions, including hypertension, heart disease, stroke and diabetes, and increases the risk of car accidents and workplace injury from drowsiness and reduced alertness.
CPAP machines work by delivering constant air pressure through the nose or mouth to keep the upper airway open during sleep. “CPAP adherence remains a major challenge,” said Tasali. “It’s estimated that about half of patients are not adherent to therapy.”
Patients often unintentionally remove their CPAP devices during the night, likely due to discomfort. Telling patients that four hours of CPAP use per night constitutes adequate treatment for their sleep apnea is “arbitrary and misleading,” Tasali said.
“This guidance remains in common use today, despite a lack of strong evidence showing that it’s sufficient or has clear benefits for health outcomes,” she said.
Unlike other therapies—such as medications—that continue to treat a health problem for hours after delivery, CPAP treatment is only effective while it is in use during sleep. That means four hours of CPAP wear might be an adequate “dose” for a patient who sleeps just four hours, but someone who sleeps for eight hours is getting the equivalent of a half-dose of treatment.
“The goal for therapy should be using the device for 100{38557cf0372cd7f85c91e7e33cff125558f1277b36a8edbab0100de866181896} of the time you spent in bed sleeping,” said Tasali. “By integrating a wearable sleep tracker, our tool provides a personal dose for CPAP therapy and a more meaningful metric for adherence monitoring that can be implemented into clinical guidelines.”
A new wearable system for tracking CPAP use
For the study, the Northwestern University team led by Bonnie Spring, Ph.D., and Angela Pfammatter, Ph.D., Professors of Preventive Medicine, modified a weight-loss app they developed that tracks diet, physical activity and weight.
To support weight loss, the mobile technology system integrates information from a wearable sleep and activity tracker and weight scale. Since excess weight is a major risk factor for sleep apnea, the investigators modified the app to have it chart patients’ CPAP wear time and check it against a goal of wearing the device for 100{38557cf0372cd7f85c91e7e33cff125558f1277b36a8edbab0100de866181896} of time spent sleeping.
“The patients wanted to see the 100{38557cf0372cd7f85c91e7e33cff125558f1277b36a8edbab0100de866181896} goal displayed in the app as a target to reach every night,” Tasali said.
By showing progress toward a sleep goal alongside other icons that track progress toward diet, activity and weight goals, the app helps people see how making improvements in one health behavior can make it easier to make changes in others.
“That’s important,” said Spring, “because insufficient sleep, poor quality diet, physical inactivity, and overweight tend to occur together. It’s a great efficiency to have tools and strategies that can help people change multiple risk behaviors at the same time.”
Based on the patients’ feedback, the researchers added features like push notifications to remind users to wear their CPAP before bedtime. The new CPAP tracking technology could be used by physicians to deliver more comprehensive and effective sleep apnea treatment.
“Right now, it’s hard for providers to counsel the patient on how to optimally use their CPAP machine, as well as for the patient to grasp how much use is adequate every night,” Tasali said. “So, not only could this app be used as a self-management tool for patients, but also as a more accurate and personalized treatment efficacy monitoring method for healthcare providers.”
As a next step, the researchers are planning additional studies to test the tool against traditional methods for monitoring CPAP use to determine whether it improves patient adherence to therapy. In addition, Tasali hopes to study the impact of percent CPAP adherence on health outcomes such as blood pressure and sugar levels.
Angela Fidler Pfammatter et al, The Development of a Novel mHealth Tool for Obstructive Sleep Apnea: Tracking Continuous Positive Airway Pressure Adherence as a Percentage of Time in Bed, Journal of Medical Internet Research (2022). DOI: 10.2196/39489
Citation:
New mobile health technology for sleep apnea care to address individual patient needs (2022, December 5)
retrieved 6 December 2022
from https://medicalxpress.com/news/2022-12-mobile-health-technology-apnea-individual.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.








